Foot Related Conditions
Foot Ulcers & Wounds
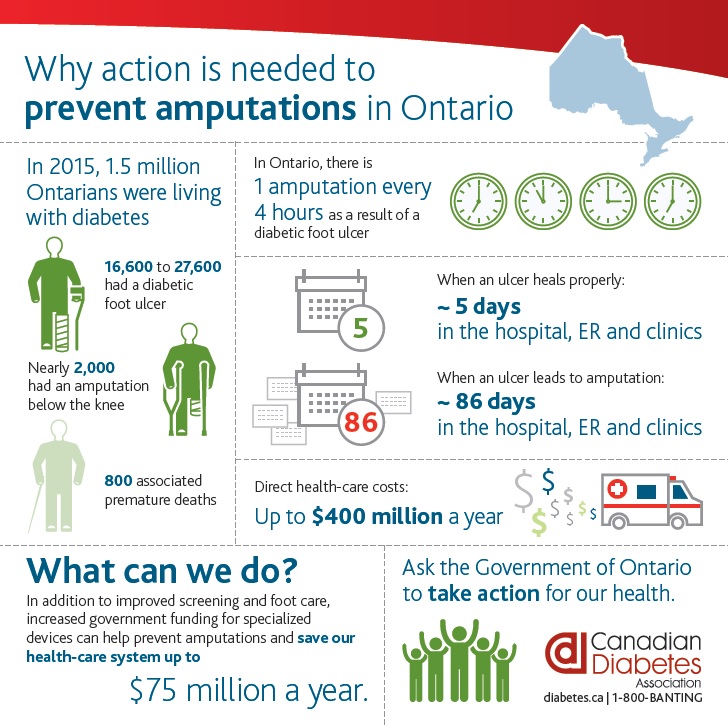
The term ulcer is used to refer to breaks in the skin. An ulcer may form due to decreased circulation or sensation within the feet. Management consists of wound evaluation, debridement, application of topical antibiotics, appropriate dressings, footwear advice, and padding or insoles and orthotics. People living with diabetes are especially prone to developing ulcers. It is vital to treat foot injuries right away.
Do you have any questions or suspect you may have an ulcer? Don’t let your foot condition worsen. Please give our office a call and have it assessed by a professional.
ul•cer
A break in the skin that is often accompanied by formation of pus and necrosis of surrounding tissue, usually resulting from inflammation or ischemia.
The Stages of Ulcers
Ulcers are skin wounds that are slow to heal and are classified into four stages, according to which layers of skin are broken through.
- Stage 1 – a reddening over bony areas characterizes ulcers in Stage 1. The redness on the skin does not go away when pressure is relieved.
- Stage 2 – blisters, peeling or cracked skin characterizes ulcers in Stage 2. There is a partial thickness skin loss involving the top two layers of the skin.
- Stage 3 – broken skin and sometimes bloody drainage characterize ulcers in Stage 3. There is a full-thickness skin loss involving subcutaneous tissue (the tissue between the skin & the muscle).
- Stage 4 – breaks in the skin involving skin, muscle, tendon and bone and are often associated with a bone infection called osteomyelitis characterizes ulcers in Stage 4.
Many different diagnostic tests can be done in the course of treating an ulcer. If the ulcer appears to be infected (i.e., there is redness and drainage), then a culture of the wound should be taken to identify the type of infection so that you can be put on the appropriate antibiotic.
If there is suspicion of the bone being infected under the ulcer, x-rays and a bone scan can be done. If there is suspicion that the underlying reason for the ulcer is poor circulation, then a non-invasive vascular study (doppler) can be done. This study is done to see if you have enough oxygen getting down to the area to heal the ulcer.
What Causes Ulcers?
Ulcers occur for different reasons, so it is imperative to determine the underlying medical problem that caused the ulcer. There are four main reasons people get ulcers on the foot.
- Neuropathic: Occurs when a patient has a loss of sensation in the feet. It is commonly seen in people with diabetes, but it can be caused by other reasons such as chronic alcohol abuse. These ulcers are generally seen under weight-bearing areas and often will begin as a callus or a corn.
- Arterial: Due to poor blood flow to the lower extremities, and can be very painful and is usually found on the toes, lower legs, ankle, heel, and top of the foot. They can very quickly become infected.
- Venous: Due to compromised veins. Veins are the vessels that take blood and fluid out of the legs and back up to the heart. Veins have small valves that allow blood to flow only one way, back up to the heart. The valves usually block the gravity from pulling the blood back down the legs. Sometimes the valves leak or cease to work at all. If they do not work, then the fluid pools down in the legs, causing swelling. This swelling leads to increased pressure in the venous system, producing discoloration of the leg, and eventually, this can lead to ulceration. They are commonly seen around the inside of the ankle and are slow to heal.
- Decubitus: Caused by excessive prolonged pressure on one area of the foot. The most common spot to see this type of ulcer is in a person confined to bed, and they occur on the backs of the heels.
How Does Your Body Heal?
What can the Chiropodist do?
Treat the infection. The chiropodist will thoroughly clean the wound to remove all infected tissue. Early, aggressive wound cleaning (called “debridement”) has been shown to more rapidly heal these wounds. If there is an infection, antibiotics can be prescribed. If the infection is severe, you may be hospitalized to receive intravenous antibiotics. Dressings are used to prevent further trauma, minimize the risk of infection, relieve local pain, and optimize the environment for healing.
Reduce the Pressure. Depending on the location of your foot ulcer, you may need to keep pressure off the area. This is called “offloading” and means avoiding all mechanical stress on the wound so it can heal. If there is no infection, a total contact cast may be used to relieve pressure (see below). Your chiropodist may recommend using “non-weight bearing” devices such as orthopedic shoes, crutches, a walker, a wheelchair or even bed rest. These can help healing by relieving pressure on the injured part of your foot.
Total Contact Casting system: combines the above treatments in a plaster cast that is proven to be the gold standard among most experts. It is believed to be the best method of offloading to help heal the ulcer. Read more about it here.
Magnetic Biostimulation Therapy: a combination of light and magnetic therapy to aid in the healing process. Read more about it by clicking here.
What can you do?
Simple daily footcare can prevent serious problems. According to the National Institute of Health, the following are simple, everyday steps that will help avoid serious complications:
- Take Care of Your Diabetes. Make healthy lifestyle choices to keep your blood sugar close to normal. Work with your health care team to create a diabetes plan that fits your lifestyle characteristics.
- Check Your Feet Every Day. You may not be aware of a foot problem. Check your feet for cuts, sores, red spots, swelling, or infected toenails. Checking your feet should become part of your daily routine. If you have trouble bending over to see your feet, use a plastic mirror to help. You can also ask a family member to help you. Important Reminder: Be sure to call your doctor immediately if a cut, sore, blister, or bruise on your foot does not heal after one day.
- Wash Your Feet Every Day. Wash your feet in warm, NOT HOT, water. Do not soak your feet because your skin will get dry. Dry your feet well. Be sure to dry between your toes. Use talcum powder to keep the skin dry between the toes and rub a thin coat of skin lotion or cream on the tops and bottoms of the feet.
- Trim your Toenails Each Week or When Needed. Trim your toenails with clippers after you wash and dry your feet. Trim the toenails straight across and smooth them with an emery board or nail file. DO NOT cut into the corners of the nail or rip off hangnails. If your nails are thick or yellowed, DO NOT cut them yourself, have a chiropodist trim them.
- Wear Shoes and Socks At All Times. Wear shoes and socks at all times. Do not walk barefoot, not even indoors. It is extremely easy to step on something and hurt your feet. Always wear seamless socks, stockings, and nylons with your shoes to help avoid the possibility of blisters and sores developing. Wear shoes that fit well and protect your feet.
- Be More Active. Walking, dancing, swimming, and bicycling are good forms of exercise that are easy on the feet. Avoid all activities that are hard on the feet, such as running and jumping.
Do you have any questions or suspect you may have an ulcer? Don’t let your foot condition worsen. Please give our office a call and have it assessed by a professional.
Visit our blog for more information on Causes, Symptoms and Treatment Options for Foot Ulcers and Wounds.
Articles of Interest
What’s in a Wound?
A foot ulcer or wound is a common complication .....
November is Diabetes Awareness Month
November is Diabetes Awareness month so let’s educate ourselves .....
Worrisome Wounds
Diabetic foot wounds and ulcers are a leading cause .....

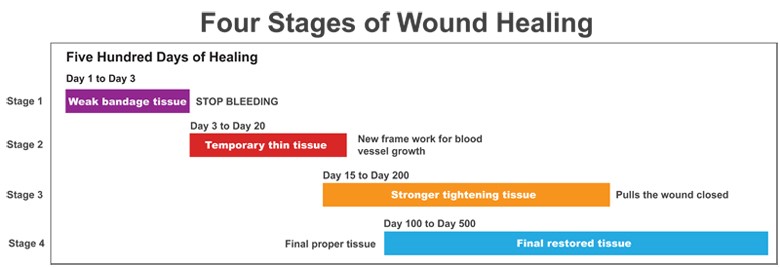

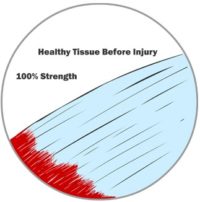
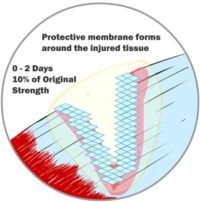 Whether it’s skin, cartilage, a tendon, a ligament, or a muscle, when we injure ourselves, we have typically caused our tissue to tear. Perhaps a little bit, perhaps a lot. The injury or wound can affect a small or large area. Immediately upon wounding soft tissue, our body’s fluids (blood, lymph and other fluids) leak from the broken tissue. The body quickly springs into action and tries to patch the leaks and contain the damage. Your body builds thin membranes around the injury to stop the bleeding. This is the very start of the healing process. Depending on the severity of the injury, this process can take minutes to hours to a few days. Think about how fast the bleeding can stop if you cut your skin. That’s how fast your body reacts to start the healing process.
Whether it’s skin, cartilage, a tendon, a ligament, or a muscle, when we injure ourselves, we have typically caused our tissue to tear. Perhaps a little bit, perhaps a lot. The injury or wound can affect a small or large area. Immediately upon wounding soft tissue, our body’s fluids (blood, lymph and other fluids) leak from the broken tissue. The body quickly springs into action and tries to patch the leaks and contain the damage. Your body builds thin membranes around the injury to stop the bleeding. This is the very start of the healing process. Depending on the severity of the injury, this process can take minutes to hours to a few days. Think about how fast the bleeding can stop if you cut your skin. That’s how fast your body reacts to start the healing process.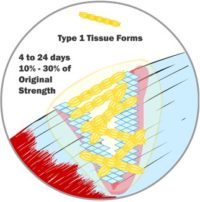
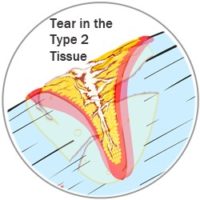
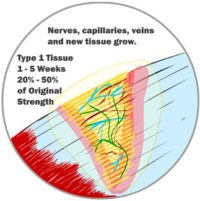 Invariably, when an injury occurs, a gap is left between the two sides of the wound. At first, it may be filled with bodily fluids, but it needs to be filled with new tissue. However, new muscles, skin, tendons, etc., don’t grow back right away. Those special tissues need nerves and blood flow to grow and work properly. In the case of a wound injury, your body first fills the gap with a special kind of tissue (we’ve simplified it and called it Type 1 tissue here). It is a generic tissue. If the wound is a cut on your skin, it is the soft pink tissue that you see right after the scab comes off. The same Type 1 tissue fills the gap regardless of what kind of tissue was injured. It is stronger than the membrane that sealed the injury in the first few hours but is not very strong. Type 1 tissue can fill a significant gap, and once Type 1 tissue is in place, new capillaries, veins and nerves can grow in and around the new tissue. These systems will be needed for the next stage in wound healing. Type 1 tissue can start forming in as little as 12 hours after your initial injury, but it does most of its growth between 4 and 24 days after injuring yourself. By the end of this stage of healing, you likely feel little to no more pain, and your injured body is at about 50% of its original strength.
Invariably, when an injury occurs, a gap is left between the two sides of the wound. At first, it may be filled with bodily fluids, but it needs to be filled with new tissue. However, new muscles, skin, tendons, etc., don’t grow back right away. Those special tissues need nerves and blood flow to grow and work properly. In the case of a wound injury, your body first fills the gap with a special kind of tissue (we’ve simplified it and called it Type 1 tissue here). It is a generic tissue. If the wound is a cut on your skin, it is the soft pink tissue that you see right after the scab comes off. The same Type 1 tissue fills the gap regardless of what kind of tissue was injured. It is stronger than the membrane that sealed the injury in the first few hours but is not very strong. Type 1 tissue can fill a significant gap, and once Type 1 tissue is in place, new capillaries, veins and nerves can grow in and around the new tissue. These systems will be needed for the next stage in wound healing. Type 1 tissue can start forming in as little as 12 hours after your initial injury, but it does most of its growth between 4 and 24 days after injuring yourself. By the end of this stage of healing, you likely feel little to no more pain, and your injured body is at about 50% of its original strength.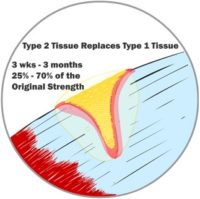
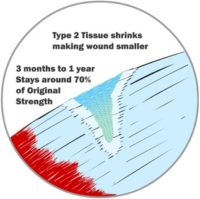 After new blood flow and nerves are in the area, the Type 1 tissue is replaced by a new Type 2 tissue. This second type of tissue is much stronger with access to proper nutrients from a regular blood supply. It bonds tightly to the ends of your wound and, over time, acts like a tightening muscle and pulls the edges of your wound together. This closes the wounded area, making it much smaller. On your skin, you see this Type 1 tissue replaced by Type 2 tissue as your scar changes from pink to much paler. The colour changes because it’s different tissue. As the Type 2 tissue pulls the wound together, we see this as the scar shrinking or fading. If the injury is under your skin, the same thing is happening; you just don’t see it. This Type 2 tissue is stronger than Type 1.
After new blood flow and nerves are in the area, the Type 1 tissue is replaced by a new Type 2 tissue. This second type of tissue is much stronger with access to proper nutrients from a regular blood supply. It bonds tightly to the ends of your wound and, over time, acts like a tightening muscle and pulls the edges of your wound together. This closes the wounded area, making it much smaller. On your skin, you see this Type 1 tissue replaced by Type 2 tissue as your scar changes from pink to much paler. The colour changes because it’s different tissue. As the Type 2 tissue pulls the wound together, we see this as the scar shrinking or fading. If the injury is under your skin, the same thing is happening; you just don’t see it. This Type 2 tissue is stronger than Type 1.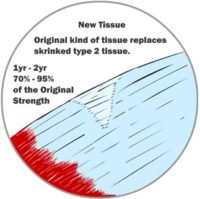
 Finally, after the wound has been shrunk as much as possible, your body replaces the Type 2 tissue with the original tissue type that was first injured. Only now does new skin, ligament, tendon, muscle, or cartilage grow. It is after your body replaces the Type 2 tissue with the original cells that your wound is considered fully healed. Only now, it regains the same kind of functionality it once had. This stage can be 1 to 2 years after the original injury though. This is the stage where the scar on your skin seems to disappear entirely. The new tissue isn’t perfect, though. The growth lines probably don’t align perfectly with the lines the old tissue took, so it will never be 100% the same. It can be pretty darn close, though. The important thing is that when the Type 2 scar tissue is replaced by normal tissue, that tissue’s function can also return substantially. Now the healing process is complete.
Finally, after the wound has been shrunk as much as possible, your body replaces the Type 2 tissue with the original tissue type that was first injured. Only now does new skin, ligament, tendon, muscle, or cartilage grow. It is after your body replaces the Type 2 tissue with the original cells that your wound is considered fully healed. Only now, it regains the same kind of functionality it once had. This stage can be 1 to 2 years after the original injury though. This is the stage where the scar on your skin seems to disappear entirely. The new tissue isn’t perfect, though. The growth lines probably don’t align perfectly with the lines the old tissue took, so it will never be 100% the same. It can be pretty darn close, though. The important thing is that when the Type 2 scar tissue is replaced by normal tissue, that tissue’s function can also return substantially. Now the healing process is complete.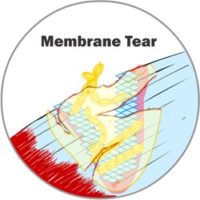
 People rarely let their bodies fully heal. Sometimes people have no choice; sometimes, people don’t know better. When you are injured, your body must go through the above process. There is no shortcut. All these stages take place, and they all take time. They take a long time. Regardless, people tend to overstrain their injury before it has healed sufficiently and constantly re-injure themselves. You’re re-injuring yourself every time you feel that ‘pain.’ You move a certain way and feel the pain, or you go about life, and the pain creeps back. You’ve undone some of the healing process every time you feel pain. Every time you feel pain, it’s because you’ve broken the membrane or torn the Type 1 or Type 2 tissue, and your body has to start the healing process for that tissue all over again. If you injure yourself badly enough each time or often enough, the amount of damage you do entirely undoes the healing your body has done, and you never get better. The injury worsens for people who never give their bodies a chance.
People rarely let their bodies fully heal. Sometimes people have no choice; sometimes, people don’t know better. When you are injured, your body must go through the above process. There is no shortcut. All these stages take place, and they all take time. They take a long time. Regardless, people tend to overstrain their injury before it has healed sufficiently and constantly re-injure themselves. You’re re-injuring yourself every time you feel that ‘pain.’ You move a certain way and feel the pain, or you go about life, and the pain creeps back. You’ve undone some of the healing process every time you feel pain. Every time you feel pain, it’s because you’ve broken the membrane or torn the Type 1 or Type 2 tissue, and your body has to start the healing process for that tissue all over again. If you injure yourself badly enough each time or often enough, the amount of damage you do entirely undoes the healing your body has done, and you never get better. The injury worsens for people who never give their bodies a chance.